Most practices still treat the revenue cycle as something that happens after a patient is seen. But by then, denials, write-offs, and patient confusion are already baked in.
At DrBillerz, we flipped the model:
👉 We run verification and cost estimation the same day a patient books an appointment.
That single shift transformed outcomes across 12+ practices:
- Patient statements < 2%
- Patient A/R ≈ 0
- Write-offs ≈ 0
The Problem With “Wait Until Check-In”
- Check-in is chaos. Patients are in a hurry, staff are multitasking, and eligibility checks are rushed.
- Estimates are guesses. Without contracted-rate data, front desks either under-collect (leading to statements) or over-collect (leading to refunds).
- Denials are planted. Referral or prior-auth requirements are discovered after the visit, not before.
The DrBillerz Approach
1. Same-Day Verification at Scheduling
When the patient calls, we verify eligibility and benefits on the spot: effective dates, deductible status, coinsurance, referral flags.
2. Contracted Rate Database
We don’t guess. We pull the actual contracted rate for that provider and service, and calculate the true time-of-service (TOS) collection.
3. Patient Financial Snapshot
Patients are given a clear estimate: “Here’s what today will cost you.”
No surprises, no confusing statements later.
4. Front-End + Back-End Handshake
Schedulers, front desk, and billers work off the same script and ticket system. Open items (e.g., PA pending) have an owner and a deadline.
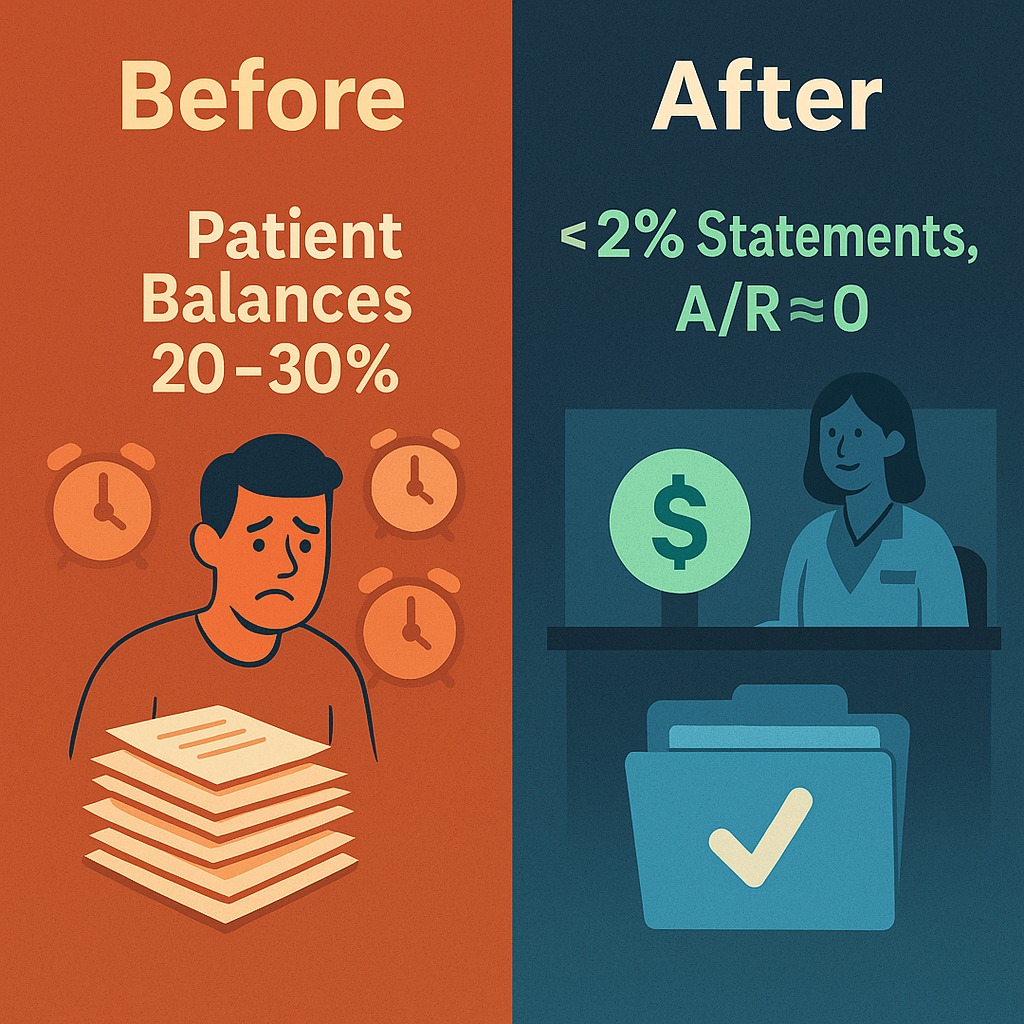
Case Study: From Statements to <2%
A multi-specialty clinic used to collect copays at check-in and send statements weeks later. The result:
- 20–30% of visits turned into patient balances.
- AR staff spent hours chasing calls and mailing reminders.
- Write-offs piled up when balances were never collected.
After switching to DrBillerz’ same-day verification + contracted rate workflow:
- Statements dropped below 2% (patients paid the right amount upfront).
- Patient AR and write-offs nearly disappeared.
- Providers saw more cash at time of service, and less patient frustration.
Why This Works
Because it’s not just tech. It’s communication:
- Front-end confirms benefits and collects with confidence.
- Back-end supports with payer rules and contracted data.
- Both sides share one ticket system, so nothing slips.
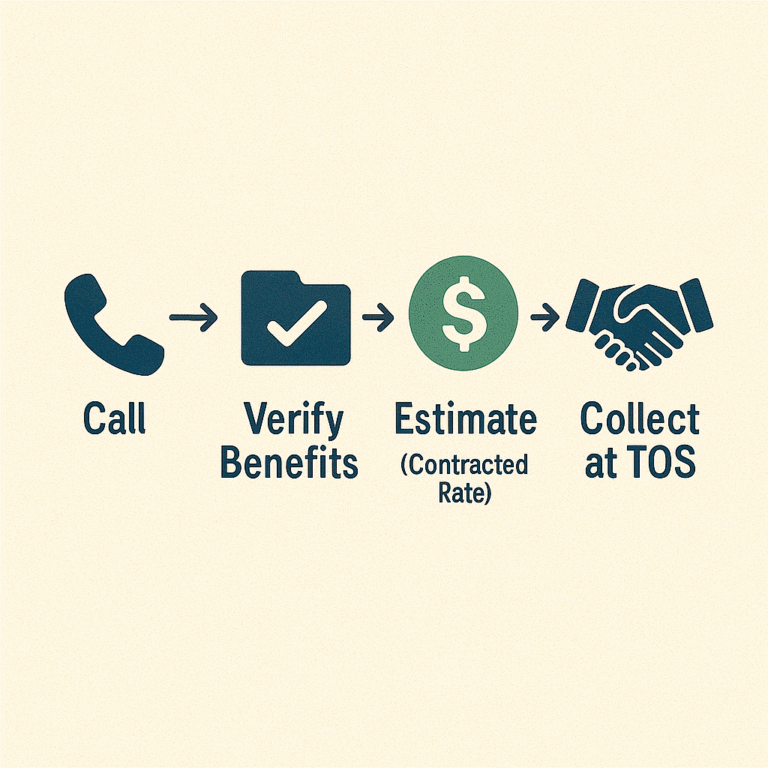
Visuals to Support the Blog
- Hero Graphic (already made):
“RCM starts when the patient calls” → Call → Verify → Estimate → Collect → AR ≈ 0 - Case Study Graphic:
Before vs After chart:
- Before: 20–30% patient balances, AR staff overloaded
- After: <2% statements, AR ≈ 0, write-offs ≈ 0
- Workflow Snapshot:
Simple 3-step visual:
📞 Call → ✅ Verify → 💲 Estimate (contracted rate) → 🤝 Collect
Final Takeaway
Revenue cycle isn’t back-office cleanup.
It’s a frontline habit that starts at the very first phone call.
When you verify and estimate upfront — using contracted rates, not guesses — patient AR disappears, statements shrink, and trust grows.
At DrBillerz, we’ve proven this across 12+ practices. And we can help you do the same.